The Quiet Corner of Health No One Talks About—But Should
Have you ever gone for a run, sneezed unexpectedly, or laughed with friends only to feel that telltale leak? Maybe you’ve noticed you plan your errands around bathroom locations, or you wake up multiple times at night to use the toilet. If so, you’re not alone. For many women, these are familiar experiences after 40.
And yet—most don’t talk about it. A study in the Journal of Women’s Health found that nearly 1 in 2 women over 40 experiences some form of urinary incontinence, but less than half ever mention it to a doctor. Instead, it’s brushed aside as “just aging” or “something we have to live with.”
The truth? These changes are common but not inevitable. And with the right knowledge, small daily habits, and sometimes professional guidance, urinary and pelvic health can be greatly improved.
Pelvic wellness isn’t just about bladder control - it’s about freedom, confidence, intimacy, and vitality. When you care for your pelvic floor and urinary system, you gain energy for the things you love, whether that’s hiking, dancing, or playing with grandchildren.
Pelvic and urinary health is a vital part of overall wellness, impacting everything from mobility and comfort to intimacy and confidence. Yet it’s still one of the most under-discussed areas of women’s health. This article explores why these changes happen, the most common concerns women face, and practical steps you can take—from nutrition to movement to daily habits—to support your pelvic health and reclaim freedom in your body.
Why Pelvic & Urinary Health Shifts After 40
By the time women reach midlife, several overlapping factors begin to influence urinary and pelvic health:
Hormonal Changes Estrogen helps keep bladder and urethral tissues elastic, thick, and well-lubricated. As levels drop during perimenopause and menopause, the tissues of the bladder and urethra become thinner, drier, and less elastic. This can make the urinary tract more prone to irritation and infection.
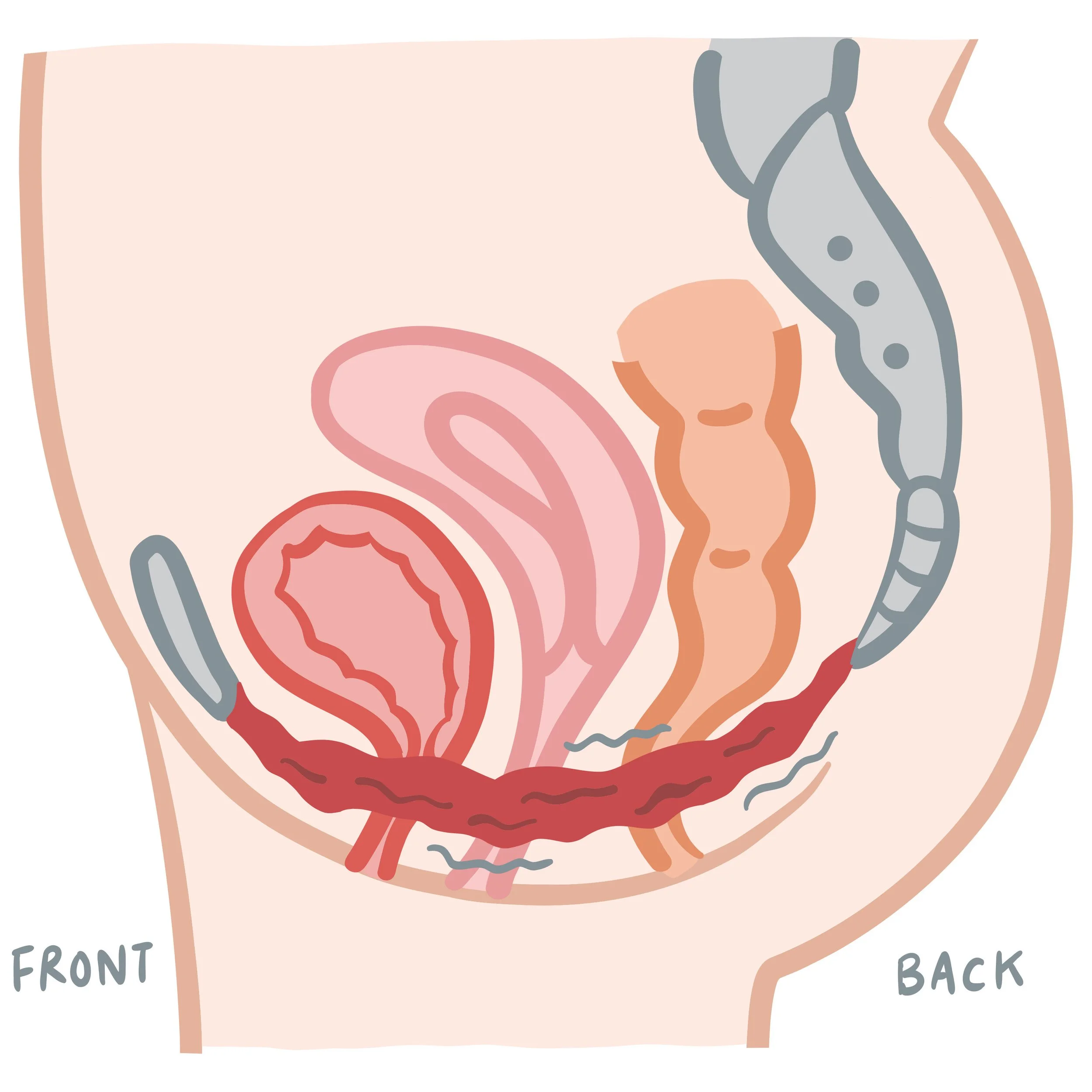
Pelvic Floor Muscle Weakness The pelvic floor is a hammock of muscles that supports the bladder, uterus, and rectum as shown by the concave area in the diagram. Over time - and especially after childbirth or years of strain - they may weaken. Weak muscles can lead to leaks, urgency, or even prolapse.
Childbirth Legacy Even decades after giving birth, women may experience the “long tail” of pregnancy and delivery—stretching, scar tissue, or nerve changes that affect pelvic function.
Natural Aging of Tissues Just like muscles elsewhere in the body, the pelvic floor can lose tone with age if not actively supported. Connective tissues gradually lose collagen and elasticity, just like skin does. This makes the bladder less stretchy and the urethra less able to seal tightly which can cause urgency and more frequent bathroom trips.
Weight and posture: Extra abdominal weight and misalignment in the spine or hips can place additional stress on the pelvic floor.
Lifestyle & Environmental Factors Years of habits like heavy lifting or high impact exercise can tax pelvic muscles as can chronic constipation (from a low fiber diet) which adds downward strain on the pelvic floor. Smoking also affects pelvic structures as it reduces circulation, irritates the bladder, and weakens collagen.
Together, these factors may affect bladder control, comfort, and pelvic stability. But with attention and consistent care, many women, and men, experience significant improvement - even after years of frustration.
Common Concerns Women Face
The urinary tract plays a crucial role in filtering waste, regulating hydration, and maintaining balance within the body. For women over 40, pelvic health becomes even more intertwined with quality of life. Issues such as weakened pelvic floor muscles, hormonal changes, or chronic dehydration can make women more vulnerable to:
Urinary Incontinence Bladder urgency or frequency is often linked to reduced elasticity or weakened muscle support. These symptoms may start small—just a drop or two—but can become disruptive over time. The social and emotional impact is real: women often avoid exercise classes, long car rides, or even laughing freely with friends. There are three types of urinary incontinence:
Stress incontinence: leakage when coughing, sneezing, laughing, or exercising.
Urge incontinence: a sudden, powerful need to urinate with little warning.
Mixed incontinence: a combination of both.
Recurrent UTIs Urinary tract infections are caused by bacterial overgrowth in the urinary tract. As estrogen declines, the protective bacteria in the vagina and urinary tract decrease reducing protective bacteria that normally helps defend against infection making infections more likely. Recurrent UTIs are more than an annoyance - they can lead to long-term bladder sensitivity if untreated.
Pelvic Floor Dysfunction & Prolapse When the muscles of the pelvic floor weaken, the organs they support may shift downward, causing pressure or a sensation of “something falling.” Women describe this as heaviness, bulging, or pressure in the vaginal area, leading to difficulty emptying the bladder, or discomfort during intimacy. In this instance, the pelvic structures need more muscular support.
Pelvic Pain or Discomfort Lower estrogen levels affect vaginal tissue health causing dryness and irritation. Pelvic pain can also come from tension, scar tissue, or nerve sensitivity. Emotional stress, past trauma, or simply holding tension in the body may also contribute. Because the pelvis holds both physical and emotional tension, addressing both body and mind can bring relief.
Men Experience Urinary & Pelvic Health Concerns Too
These concerns are most often driven by prostate conditions, pelvic floor muscle dysfunction, and age-related changes.
Men can develop various types of urinary incontinence, with stress incontinence typically following prostate surgery or pelvic muscle weakness, and urge incontinence also being common. Treatments for prostate cancer may also damage nerves or muscles necessary for bladder control, leading to further urinary problems.
Pelvic floor dysfunction is another challenge, contributing to urinary and bowel difficulties, pelvic pain, and sexual health issues such as erectile dysfunction. While urinary tract infections are less frequent in men, they still occur and are often linked to prostate or bladder conditions. Other issues affecting men’s urinary health include bladder stones, bladder cancer, bowel incontinence, and neurologic disorders (like Parkinson’s disease, stroke, or diabetes).
Symptoms often include frequent urination, urgency, incomplete bladder emptying, nighttime urination, pelvic discomfort, and leakage. Contributing factors range from aging and prostate enlargement to constipation, obesity, medications, heavy activity, chronic coughing, and pelvic injuries.
Awareness is the first step — and the second is using nutrition and daily practices to build a foundation of support.
Both women and men can support their urinary and pelvic health through the diet and movement suggestions that follow. In addition, men should also focus on consuming lycopene-rich foods and omega-3 fatty acids to support their prostate health.
Nutrition is one of the most overlooked but powerful tools for pelvic and urinary health. The foods you eat influence not only hydration and digestion but also inflammation, the microbiome, and tissue integrity. Let’s break it down:
Hydration: More Than Just Drinking Water
Aim for 6–8 cups of water spread throughout the day, not “chugging” large amounts at once. Too much water all at once overwhelms your body and it cannot be readily absorbed so it ends up being peed away increasing the chance for leaks. Too little water on the other hand concentrates the urine which can irritate the bladder lining.
Reduce fluids 2 hours before bed to limit nighttime bathroom trips and disrupted sleep. Aim to get the majority of your hydration early in the day.
Good quality filtered water or mineral water supports hydration without extra irritants. Infuse with cucumber, berries, watermelon, or herbs for gentle flavor without irritation.
Avoid “just in case” trips to the bathroom - this trains your bladder to signal urgency more often than necessary.
Herbal Teas (Caffeine-Free) are soothing and hydrating, without the irritation of regular tea or coffee.
Choose Foods That Nourish the Bladder & Pelvic Tissues
High-Fiber Foods in a fiber-rich diet support digestion and prevent constipation which can add pressure to the pelvic floor and bladder. Good sources include: whole grains (oats, barley, brown rice, quinoa, and farro), legumes (lentils, chickpeas, black beans), fruits (pears, apples, prunes, bananas, blueberries, and strawberries), and vegetables (leafy greens, carrots, squash, beets, cabbage).
Collagen & Vitamin C–Rich Foods support the strength and flexibility of the pelvic floor muscles and connective tissues. Some foods like bone broth, chicken skin, and fish with skin are good sources of collagen while other foods rich in vitamin C like citrus, bell peppers, strawberries aid in collagen production.
Magnesium & Calcium Rich Foods help relax muscles to ease urgency and calm bladder spasms. They may aid in the prevention of kidney stones. Try pumpkin seeds, almonds, spinach, black beans, whole grains, and avocado.
Prioritize Prebiotic, Probiotic, & Fermented Foods which help protect against UTIs by supporting healthy gut and vaginal microbiomes. Prebiotics found in onions, garlic, asparagus, leeks, oats, and bananas feed the healthy bacteria that are found in fermented foods and called probiotics. Try to incorporate a variety of fermented foods such as kefir, yogurt with live cultures (and minimal added sugar), sauerkraut, kombucha, kimchi, and miso into your diet daily.
Anti-Inflammatory Foods help reduce chronic bladder irritation and inflammation that can cause bladder sensitivity and discomfort. They also provide antioxidants that combat oxidative stress and protect the bladder tissues from damage. Examples of food to eat include fatty fish (salmon, sardines), healthy fats (olive oil, walnuts, flaxseeds), berries (especially blueberries and blackberries), cruciferous vegetables (broccoli and cauliflower), leafy greens (kale and spinach), green tea, and turmeric.
Plant-Based Phytoestrogens are natural compounds that structurally mimic estrogen and can provide light hormonal support to help maintain bladder tissue health. Good sources include flaxseeds, soy (tofu, tempeh, edamame), sesame seeds, and lentils.
Herbs for Bladder Calm: parsley, dill, fennel, coriander, chamomile.
Foods to Approach with Caution
These foods they may irritate the bladder. Not everyone reacts the same way so the key is to track your personal triggers rather than eliminating everything at once. Try keeping a bladder diary for a week and track what you eat and when symptoms appear - patterns often become clear.
Caffeine stimulates urgency: coffee, black tea, energy drinks.
Alcohol is a diuretic that irritates tissues: especially wine and beer.
Carbonated drinks increase bladder pressure: soft drinks, sparkling water, and champagne.
Spicy Foods like chili peppers, hot sauces.
Excess Citrus and their juices are especially acidic and irritating: oranges, grapefruits, lemonade (in moderation is often fine).
Artificial Sweeteners such as aspartame and saccharin found in diet sodas, sugar-free gum, and “diet” foods can provoke bladder symptoms.
Highly Processed Foods whose preservatives and additives can sometimes irritate the bladder.
Lifestyle Practices Beyond the Plate
Nutrition works best when paired with supportive daily practices:
Pelvic Floor Exercises (Kegels) Considered the gold standard for strengthening the pelvic floor, it’s important to do them correctly.
How to do them right: Imagine gently stopping urine midstream (though don’t actually practice on the toilet). Lift and hold for 3–5 seconds, then relax fully.
Release matters as much as strength: Constant clenching can create tension and pain. Balance strengthening with relaxation.
Beyond Kegels
Gentle yoga: child’s pose, happy baby, supported squats, and bridge pose focus on deep core strength, alignment, and pelvic floor balance.
Breathwork: diaphragmatic breathing trains the pelvic floor to work in sync with the diaphragm.
Glute and hip strengthening: bridges, clamshells, squats—all help stabilize the pelvis.
Postural awareness: Sitting slouched or standing with poor alignment strains the pelvic floor.
Mindful Daily Movement: Walking, stretching, and resistance training all improve circulation, digestion, and pelvic support. Avoid sitting for long stretches without moving and use proper lifting techniques by bending your knees and not your back.
Restorative Sleep: Adequate sleep helps regulate hormones that influence bladder health.
Stress Management: High stress tightens pelvic muscles which can increase urgency, pain, and frequency; practices like meditation, breathwork, or tai chi can help. Diaphragmatic breathing calms the nervous system and helps release pelvic tension.
Balanced Bathroom Habits: Avoid “just in case” trips to the bathroom too often, which can actually train the bladder to signal urgency unnecessarily. Don’t rush urination taking the time to empty the bladder fully. Avoid holding urine for long periods, which can weaken bladder muscles and promote infection.
Quit Smoking: Smoking increases coughing and bladder irritation, heightening leakage risk. Quitting benefits overall health and reduces incontinence.
Morning: Drink a glass of water, do 5 minutes of pelvic floor awareness breathing.
Daytime: Walk or stretch regularly; avoid sitting for hours without movement.
Meals: Choose fiber-rich foods to prevent constipation and include a probiotic option daily.
Evening: Cut back on fluids two hours before bed, practice gentle yoga or relaxation.
Weekly: Include resistance training 2–3 times per week, balanced with yoga or Pilates.
When to Seek Professional Help
There’s no reason to “just live with it.” Professional support can make all the difference. Some signs mean it’s time to go beyond home care:
Leaks happening daily or limiting your lifestyle.
Waking multiple times a night to urinate.
Pain, burning, or discomfort that persists.
Recurrent UTIs (more than 2–3 per year).
Sensation of heaviness or bulging in the vaginal area.
Specialists who can help:
Gynecologists or urogynecologists.
Urologists.
Pelvic floor physical therapists (one of the most effective interventions).
Health coaches/nutritionists for integrative lifestyle support.
Seeking help isn’t a failure—it’s a step toward freedom and healing.
Breaking the Stigma
Perhaps the biggest challenge women face with urinary and pelvic health isn’t the symptoms—it’s the silence. Too often, women dismiss symptoms as “just getting older” or feel embarrassed to mention them—even to their doctor. But speaking openly about pelvic health is empowering.
Sharing experiences with friends normalizes the conversation. Talking to a healthcare provider opens doors to effective solutions. And taking action—whether through food, movement, or professional care—restores confidence and joy in daily life. Pelvic wellness is about living fully, not just symptom management.
Pelvic and urinary health after 40 may feel like an uncomfortable subject, but it’s a vital part of living well. From incontinence to recurrent infections to pelvic floor weakness, these issues are common—but they are not inevitable.
By supporting your body with nourishing foods, smart hydration, gentle strengthening, and daily mindful habits, you can protect and even improve your pelvic health at any age. And remember: reaching out for help is not a sign of weakness, but a step toward freedom.
Caring for your pelvic health is about more than preventing leaks or discomfort—it’s about reclaiming confidence, intimacy, and the simple joy of moving through the world without worry.
Let’s get cooking!
Cooking isn’t just about flavor—it’s a way to actively support your body. By choosing ingredients rich in fiber, minerals, and hydration, you can ease pressure on the pelvic floor, encourage healthy digestion, and help your urinary system function smoothly. Simple, everyday meals can be a powerful tool for long-term wellness.
Kefir Breakfast Bowl
This Kefir Breakfast Bowl is as beautiful as it is beneficial. A creamy base of probiotic-rich kefir is topped with fresh fruit, fiber-packed flaxseed, crunchy granola, and magnesium-rich pumpkin seeds. Together, these ingredients create a satisfying and energizing meal that supports both digestive balance and urinary health.
Whether you customize it with seasonal fruit, warming spices, or savory toppings, this bowl offers a deliciously simple way to care for your pelvic and urinary wellness while starting the day on a nourishing note.

Kefir Breakfast Bowl
Ingredients
- 1 cup plain kefir (unsweetened, with live cultures)
- 1/2 cup fresh berries (blueberries, blackberries, and/or raspberries)
- 1/2 small banana, sliced
- 1/3 cup homemade sourdough granola (or store-bought low-sugar granola)
- 1 tbsp ground flaxseed or chia seed
- 1 tbsp pumpkin seeds (pepitas)
- 1 tsp raw honey or pure maple syrup (optional)
- 1/2 tsp chai spice blend or ground cinnamon
- fresh mint leaves for garnish (optional)
Instructions
- Pour the kefir into a bowl and top with the fresh fruit.
- Sprinkle with the granola, flaxseed, and pumpkin seeds.
- Drizzle with the honey or maple syrup if desired and lightly dust with the chai spices or cinnamon.
- Finish by garnishing with a few fresh mint leaves. Serve immediately.
Notes
Four flavorful variations for flexibility and seasonal inspiration:
- Top the plain kefir with fresh pineapple, mango, kiwi, toasted coconut flakes, chia seeds, a squeeze of lime and a drizzle of honey for a tropical twist.
- Blend the kefir with a spoonful of pumpkin puree and top with diced apples and pear, spiced pecan granola, flaxseed, and a sprinkle of cinnamon and nutmeg for fall flavors.
- Blend the kefir with roasted beet puree and top with berries, pumpkin seeds, and cacao nibs for an antioxidant rich treat.
- Make it savory by seasoning the kefir with salt and pepper and then topping it with diced cucumber, cherry tomatoes, avocado, sunflower seeds, fresh dill, and a drizzle of olive oil and a sprinkle of za'atar or oregano.
Chickpea, Lentil, & Broccoli Salad with Orange Tarragon Vinaigrette
Chickpea, Lentil, and Broccoli Salad with Orange-Tarragon Vinaigrette brings together hearty chickpeas, earthy lentils, and lightly steamed broccoli, all tossed in a bright orange–tarragon vinaigrette. The citrus lends a fresh lift, while tarragon adds subtle anise notes that complement the legumes beautifully. Packed with fiber, plant-based protein, and magnesium-rich ingredients, this dish not only satisfies but also supports digestive ease and muscular balance—two essential allies in maintaining pelvic and urinary health. The combination of legumes and greens nourishes gut and bladder function, while the light, aromatic dressing makes it a refreshing option for lunch or dinner.

Chickpea, Lentil, & Broccoli Salad with Orange Tarragon Vinaigrette
Ingredients
- For the Orange-Tarragon Vinaigrette:
- 3 tbsp extra virgin olive oil
- 3 tbsp fresh orange juice
- 1/3 c red wine vinegar
- 1 1/2 tsp orange zest
- 1 tbsp fresh tarragon, finely chopped (or 1 ½ tsp dried)
- ⅛ tsp chipotle powder (optional)
- 1 teaspoon Dijon mustard
- For the Salad:
- 2 cups packed chopped kale
- 1 cup cooked chickpeas, (drained and rinsed if canned)
- 1 cup cooked green or black lentils
- 2 cups broccoli florets, blanched or lightly steamed
- 1 cup cherry tomatoes, halved
- 2 tbsp finely diced red onion
- 2 tbsp chopped fresh parsley
- ½ cup walnuts, toasted and roughly chopped
- ⅓ cup sundried cranberries, low or no sugar
- 4 oz crumbled feta cheese
- salt and pepper to taste
Instructions
- Make the vinaigrette in a small bowl or jar by whisking together the olive oil, orange juice, vinegar, orange zest, tarragon, chipotle powder (if using), and Dijon mustard. Season with salt and pepper to taste. Let sit for 5–10 minutes to allow the flavors to meld.
- Blanch the broccoli (optional but recommended). Bring a small pot of salted water to a boil. Add broccoli florets and cook for 1–2 minutes until bright green and just tender. Drain and transfer to a bowl of ice water to stop cooking. Pat dry.
- Put the chopped kale in a large bowl and add about 1/3 of the orange vinaigrette. Use your hands to massage the kale so it gets soft and easier to digest.
- Add the remaining ingredients and the rest of the vinaigrette to the bowl. Toss gently to combine. Taste and adjust seasoning if needed.
- Serve immediately or chill for 30 minutes for deeper flavor. Garnish with extra tarragon or orange zest if desired.
Notes
- Keeps well for 2-3 days in the fridge.
There you have it!
Remember that small, daily choices add up. A nourishing diet, hydration, mindful habits, and pelvic support practices can help women (and men!) over 40 maintain strength, comfort, and confidence well into the decades ahead.